The Dark Side of Technology: Exploring Spinal Cord Stimulator Horror Stories and Negative Outcomes
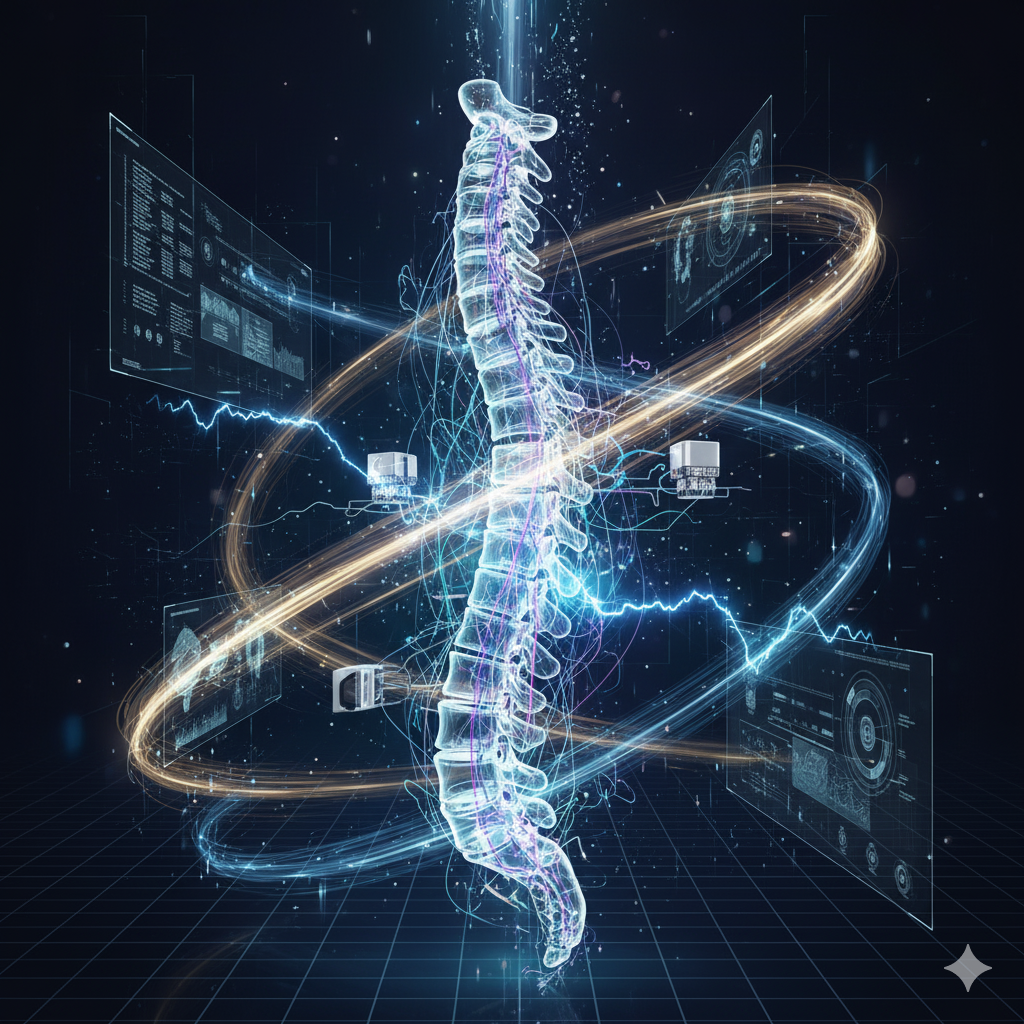
Spinal Cord Stimulators (SCS) are often presented as a revolutionary “last resort” for individuals suffering from intractable chronic pain, offering hope when traditional pharmacological and surgical treatments have failed. By delivering mild electrical impulses to the spinal cord to interrupt pain signals, these implanted devices can be life-changing for many patients. However, the patient experience is not universally positive. When searching for information on SCS, one inevitably encounters the alarming reality of spinal cord stimulator horror stories—accounts of severe complications, device failures, and debilitating outcomes that cast a shadow on this technology. These negative narratives underscore a critical truth: while SCS can be immensely successful for some, the risks involved are substantial, often leading to a cycle of pain, revision surgeries, and profound emotional distress.
Clinical data often confirms the frequency of these adverse events. Statistics suggest that complication rates can be high, with technical issues and a lack of sustained efficacy being the primary drivers for device removal (explantation). The term spinal cord stimulator horror stories frequently summarizes patient experiences of surgical trauma, chronic hardware malfunctions, and, paradoxically, an agonizing increase in pain. These accounts emphasize that the choice to implant an SCS is not a minor procedure but a permanent alteration to the nervous system and body, carrying risks that extend far beyond initial recovery and impact long-term quality of life. Understanding the scope of these failures—from device migration to life-threatening infection—is crucial for setting realistic expectations and navigating the complicated reality of chronic pain treatment.
The Leading Complications: Device Failure and Surgical Trauma
The most common issues recounted in spinal cord stimulator horror stories revolve around the mechanical stability of the implant and the immediate, inherent risks of any procedure near the delicate spinal column. These complications are frequent contributors to the high rate of surgical re-interventions.
Lead Migration and Loss of Pain Relief
The single most common device-related complication reported is lead migration. The electrical leads, or wires, are situated in the epidural space—a site that shifts naturally with body movement. Despite anchoring techniques, a significant number of patients experience lead slippage. When the leads move, the electrical stimulation shifts to unintended areas, often resulting in:
- Erratic and Painful Stimulation: Patients describe sudden, painful shocking or jolting sensations in areas previously unaffected, such as the flank, groin, or extremities, due to misplaced electrical field coverage.
- Complete Efficacy Failure: More commonly, migration leads to a total loss of effective pain coverage, leaving the patient with the original, untreated chronic pain compounded by the discomfort and bulk of the implanted hardware.
These events almost always necessitate follow-up surgery—a revision—to attempt repositioning or replacement of the leads. This cycle of re-intervention exposes patients to repeated surgical risks and prolongs their physical and emotional recovery. Data has shown that lead failure and subsequent lack of efficacy account for a significant percentage of all explant surgeries.
Neurological Damage and Spinal Fluid Leaks

The surgical placement of the leads, whether percutaneous (through a needle) or surgical (paddle lead), carries the unavoidable risk of damage to the neural structures. Although rare, accounts of severe neurological injury form the most devastating of spinal cord stimulator horror stories.
- Direct Spinal Trauma: Trauma to the nerve roots or the spinal cord itself during lead insertion can result in permanent neurological deficits, including numbness, chronic weakness, or even paraparesis (partial paralysis) below the implant site. Such outcomes fundamentally transform the patient’s disability, exchanging chronic pain for permanent motor or sensory impairment.
- Cerebrospinal Fluid (CSF) Leak: Puncturing the dura mater (the sheath surrounding the spinal cord) can cause a CSF leak. This results in severe, often debilitating, positional headaches that worsen when sitting or standing and improve only when lying down. These dural puncture headaches are agonizing and may require emergency surgical intervention, such as a blood patch, to resolve. In the worst cases, these complications become a new source of chronic suffering that persists long after the device is removed.
Biological and Systemic Horror Stories: Infection and Dysfunctional Stimulation
The body’s reaction to the foreign material is another major source of adverse outcomes, generating some of the most alarming spinal cord stimulator horror stories due to their potential for life-threatening consequences and persistent, excruciating pain.
Infection: The Explantation Imperative
Infection is the most critical biological complication and a primary driver for mandatory device removal. Rates of infection, while improving with enhanced surgical protocols, still remain a concern, reported in several percent of cases. Infections can manifest:
- At the Implanted Pulse Generator (IPG) Site: Pain, redness, swelling, or drainage around the battery site in the abdomen or buttocks is common. This can lead to skin erosion, where the hardware starts to push through the skin, causing severe local pain and requiring explantation.
- In the Epidural Space: This deep-seated infection, leading to an epidural abscess or meningitis, constitutes a surgical emergency. It requires aggressive, prolonged intravenous antibiotic therapy and the immediate explantation of the entire SCS system. The hardware acts as a protected harbor for bacteria, making sterilization impossible without removal. Such infections severely compromise the patient’s overall health and dramatically delay any further pain management treatments.
Paradoxical Pain and Intolerable Dysesthesia
The failure of the device to manage pain is often not a passive event but an active source of new pain. Many of the most heartbreaking spinal cord stimulator horror stories involve the device achieving the opposite of its intended effect.
- Worsened Pain (Hyperalgesia): Some patients report that the implantation surgery or the electrical stimulus itself triggers an unexplained increase in their pre-existing pain or the creation of entirely new pain syndromes. This “inadequate pain control” or lack of efficacy is, statistically, the most frequent reason for SCS explantation, accounting for over two-thirds of removals in some studies.
- Intolerable Paresthesia: The core mechanism of traditional SCS relies on generating a tingling sensation (paresthesia) to mask pain. However, this sensation is highly subjective. Many patients describe the tingling as aggressively uncomfortable, burning, vibrating, or feeling like repeated “jolts of electrocution” that are often more distracting and painful than the original chronic pain. While newer, paresthesia-free devices (like high-frequency or burst stimulators) have been developed, they still carry risks of discomfort and may not eliminate this adverse sensory experience for all users. The chronic rejection of the stimulation itself is a major cause for explantation.
The Explantation Trauma: A Second Surgical Nightmare
When the spinal cord stimulator fails, the only recourse is often explantation surgery—the complete removal of the leads and the battery pack. This procedure, while intended to solve the problems created by the first surgery, introduces a fresh wave of risks and trauma, often chronicled in detail within the spinal cord stimulator horror stories online.
Removing the device is rarely simple. The body forms scar tissue, known as a scar capsule or epidural fibrosis, around the implanted hardware, particularly around the paddle leads that are surgically placed. Detaching the leads from the spinal cord involves meticulous dissection and manipulation of the area, carrying a renewed risk of dural tears, nerve root damage, and post-operative bleeding (hematoma). For percutaneous leads anchored near the spine, the removal process must be conducted with extreme care to ensure no residual hardware is left behind that could migrate or cause friction against neural tissue. The recovery from this explantation surgery, though sometimes quick, is frequently complicated by persistent hardware discomfort at the original battery pocket site or by phantom-pain sensations where the stimulation used to occur. For patients, this second, major surgery for explantation is the definitive admission of defeat, often leaving them in worse physical and psychological shape than they were prior to the initial implantation.
The Emotional and Financial Burden: Unrealistic Expectations and Costly Failure
The emotional and financial fallout of a failed SCS device forms the deepest layer of the spinal cord stimulator horror stories. Patients often arrive at SCS after years of pain and failed treatments, viewing the device as their final, guaranteed solution.
The marketing surrounding SCS technology often promotes high success rates, creating expectations that are frequently shattered by the reality of long-term complication rates that hover around 30% or more. This misalignment between hope and reality can lead to severe major depression, anxiety, and feelings of helplessness when the device fails. For many, the SCS failure is the catalyst for increased suicidal ideation, given the exhaustion of perceived treatment options. The psychological damage from chronic pain is compounded by the trauma of repeated surgeries, infections, and the inability to trust their medical team.
Financially, the burden is crushing. The device and implantation can cost upwards of $35,000 to $70,000 or more. When the device fails, the patient then faces costly revision surgeries (often $15,000 to $25,000 per procedure) and the ultimate expense of explantation. Patients recount being left with massive medical debt for a piece of hardware that not only failed to alleviate their pain but actively caused new, lasting injury, perfectly illustrating the catastrophic financial aspect of these spinal cord stimulator horror stories. The regulatory environment, which often allows devices to enter the market via the 510(k) pathway (which does not require new evidence of safety and efficacy), has been criticized for prioritizing innovation speed over long-term patient protection.
CUSTOM FAQ SECTION
Why is lead migration the most common issue in spinal cord stimulator horror stories? Lead migration is the most common issue because the electrical leads of the spinal cord stimulator are placed in the epidural space, a delicate area of the spine that naturally moves and flexes with the body. Despite the use of anchors, this constant movement can cause the leads to shift away from the targeted nerve area. When this occurs, the patient experiences a sudden loss of pain relief or painful, erratic stimulation, often necessitating another surgery for repositioning.
Does a spinal cord stimulator always eliminate chronic pain? No, a spinal cord stimulator is intended to manage pain, not eliminate it. Many of the most disappointing spinal cord stimulator horror stories arise from the unrealistic expectation that the device will provide a complete cure. Clinical trials often measure success as a 50% reduction in pain. A significant portion of patients experience inadequate pain control even after a successful trial, which is the leading reason for the device’s eventual removal (explantation).
What is the risk of life-threatening infection with a spinal cord stimulator? The risk of infection, while relatively low (often cited in the single digits), is the most serious biological risk, contributing severely to spinal cord stimulator horror stories. An infection deep within the epidural space or around the implanted pulse generator can lead to a severe abscess or meningitis. If this occurs, the entire device must be surgically removed (explanted) immediately, and the patient requires intensive, long-term intravenous antibiotics to resolve the infection.
Can the electrical stimulation from the SCS actually make the pain worse? Yes. This is a common and distressing adverse outcome. Many patients report paradoxical pain or hyperalgesia, where the pain actually increases after implantation. Furthermore, the tingling sensation (paresthesia) used by traditional stimulators can be perceived as an intolerable, painful burning, buzzing, or “shocking” sensation, which is more unpleasant than the original chronic pain itself. This is a significant factor in why a patient might request the explantation of the spinal cord stimulator.
What is explantation, and why is it a risky procedure? Explantation is the surgical procedure to remove the entire spinal cord stimulator system—both the battery pack and the electrical leads. It is considered a risky procedure because the body forms scar tissue (fibrosis) around the leads in the spinal canal. Surgeons must meticulously detach these leads from the sensitive nerve roots without causing trauma, which carries a renewed risk of nerve damage, dural puncture, and prolonged surgical site pain, compounding the patient’s existing chronic pain issues.